- Phone: +91-9121106681
- Email: ardsihyd@gmail.com
Dementia Diagnosis
Most of us forget things every day. We might forget the name of the person we just met or where we placed our glasses or why we entered a room. People of all ages experience these things, although many people find they get more common with age, or they may worry more about them as they get older. However, this type of forgetfulness is not necessarily a sign of dementia.
We can also experience problems with our thinking from time to time. We might find it hard to concentrate on something we are trying to do, or struggle to follow a conversation we are having.
While it can be normal to experience difficulties from time to time, memory and thinking problems that start to have an effect on our everyday life may be a sign of something more serious. Ongoing memory and thinking problems can have many causes, including:
- • Infections
- • Vitamin deficiencies
- • An underactive thyroid
- • Stress, anxiety, and depression
- • Some medications you might be taking for other health conditions.
In some cases, however, ongoing memory, thinking and communication problems can be a sign of dementia.
Dementia affects people in different ways. As symptoms get worse and become more noticeable, family and friends may start to recognize that someone is struggling. The symptoms below could be signs of dementia, particularly if they are new and appear to be getting worse over time.
- • Short-term memory loss, which might lead to someone becoming repetitive, forgetting recent events, or finding it difficult to learn anything new.
- • Changes in ability to think things through and solve problems.
- • Losing track of the date or time.
- • Struggling to find the right words when talking.
- • Difficulty understanding instructions.
- • Making mistakes in everyday tasks.
- • Becoming withdrawn and unmotivated.
- • Other changes to behavior, personality, and mood.
- • Changes in vision, balance, and walking.
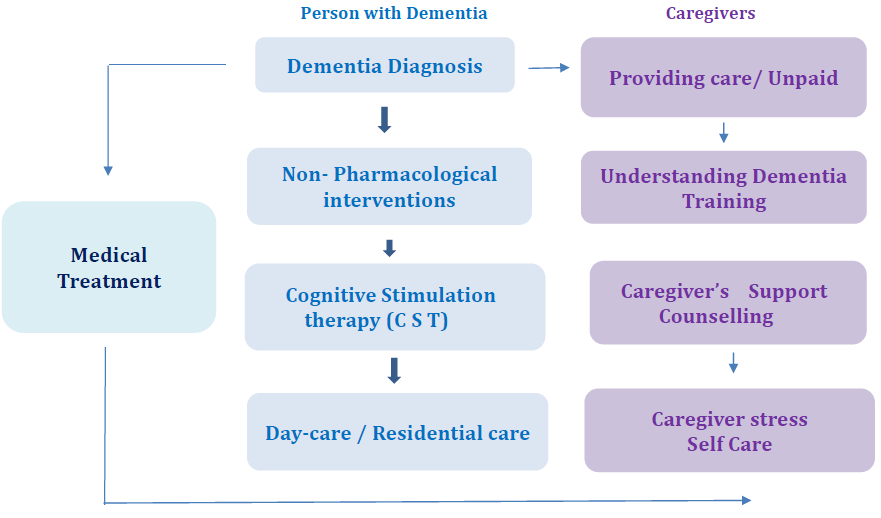
Dementia Diagnosis & Care pathway

Dementia Journey for the person living with dementia and their family caregiver
Blood Tests: There is no single blood test to diagnose dementia. A range of tests are performed to rule out underlying medical conditions that can be the reversible causes of dementia. These include:
Complete Blood Picture – to rule out any infections Thyroid Function tests – for an underactive thyroid Vitamin B12 level & Folic acid – to see for any deficiency ALT or AST levels for checking liver function Blood electrolytes and kidney function tests Glucose levels to detect diabetes HIV test to look for AIDS and also test for Syphilis.
Biomarkers: A biomarker is an indicator which could suggest whether a person has a disease, or a risk of developing it.
A biomarker can be a specific process, a molecule or protein that we can measure in the body, which informs us about a person’s health.Specific biomarkers for Alzheimer’s disease are Amyloid -Beta peptide oligomers Phosphorylated Tau Beta – Amyloid.
Neurofilament light (NFL) Glial fibrillary acidic protein (GFAP) Research is on and these tests are yet to be available at all health care centers.A lumbar puncture (spinal tap) may be performed to obtain cerebrospinal fluid, which is then analyzed for evidence of Alzheimer’s disease proteins or of certain infections, inflammatory conditions, or other diseases that may cause dementia.
Antinuclear antibodies blood test to diagnose any autoimmune diseases. C-reactive Protein & ESR. Lipid Profile – cholesterol levels Toxicology Screen – Blood and urine examination for any DRUGS and alcohol.
Brain imaging studies:
Brain imaging is a common way to diagnose dementia, and can help rule out other causes of brain damage. Computerized Tomography – CT Magnetic Resonance Imaging: Brain atrophy, strokes (large and small), ischemia, changes to blood vessels, hydrocephalus, subdural hematomas and tumors. Positron emission tomography PET scan can detect changes in glucose metabolism, presence of amyloid proteins, oxygen metabolism, and blood flow, all of which can reveal abnormalities of brain function.
Electroencephalography (EEG) is a noninvasive, cost-effective, and easy-to-use brain wave recording technique that can play a significant role in the diagnosis and classification of dementia. EEG can help diagnose and differentiate between Dementia with Lewy Bodies and Alzheimer’s Disease; it can predict the stages of dementia and determine the severity of dementia. EEG can help predict treatment response for Dementia with Lewy Bodies.Dementia as of now has no CURE only CARE. Each individual living with dementia is unique with their own tra trajectory of illness. As the condition progresses patients develop personality changes, behavioural and psychological symptoms which may require management with medications. Research has shown that along wi with medications, cognitive stimulation and rehabilitation therapies are very beneficial in helping preserve the cognitive reserve, reduce the psychological symptoms and delay the progression of dementia.
Dementia Progression:
Dementia is progressive. This means the symptoms may be mild at the beginning but get worse with time, usually several years, as the structure and the chemistry in the brain become increasingly damaged with time. How quickly dementia progresses depends on the individual – their physical make -up, emotional resilience and the kind of support available to them.
Dementia affects everyone differently. It is said to evolve in three stages, but it is important to realize that this is only a rough guide to the progression of the condition. The three stages include – Early stage, Middle stage, Later stage. These may also be called as mild, moderate or severe because this describes how much the symptoms affect a person.
Early stage – a person’s symptoms are often relatively mild and not always easy to notice. Common early-stage symptoms include problems with memory, speed of thought, language or perception. Many people at the early stage of dementia stay largely independent and only need a bit of assistance with daily living. It is important to focus on what the person can do and not to take over and do things for them. Instead, try doing things with them, for example helping the person develop a routine, reminder lists and prompts, and use technology.
The early stage of dementia is when many people choose to make plans for the future, while they still have the ability (‘mental capacity’) to do so. This includes making a Lasting power of attorney (LPA), and advance decisions and advance statements to ensure their wishes and preferences are made clear. A Lasting power of attorney (LPA) is a legal tool that lets you choose someone you trust to make decisions for you. There are two different types of LPA: property and affairs LPA and health and welfare LPA. LPAs can make things easier for you and the people you are close to as your dementia progresses.
When you have dementia, planning ahead may include writing an advance decision or advance statement or advance medical directive. You can use these to make decisions about care and treatment in the future.
Middle stage: In the middle stage of dementia, symptoms become more noticeable and the person will need more support in managing daily life. This stage of dementia is often the longest. On average it lasts about two to four years during which time symptoms are likely to develop in the following ways: Existing problems with memory and thinking, the way a person speaks or uses language and problems with orientation will become worse.
Symptoms of apathy, anxiety and depression tend to continue. Many people tend to develop delusions and hallucinations.
Changes in behavior tend to start from the middle stage of dementia. These include: Agitation and restlessness – for example, fidgeting or walking up and down, screaming or shouting. Repetitive behavior – for example, repeatedly pulling at clothes or asking the same question over and over. Following a carer around (trailing) or constantly checking that they are near. Disturbed sleep patterns – sleep is particularly disrupted,
Losing inhibitions – for example, saying things aren’t appropriate or undressing in public
People may become more agitated, aggressive or confused in the late afternoon or early evening, a pattern known as ‘sundowning’.
These behaviors are often because the person has a specific physical or emotional need (for example, hunger or boredom) that is not being met.
In all types of dementia, difficulties with using the toilet (urinary or fecal incontinence) can start at this stage.
In dementia with Lewy bodies, problems with movement are likely to get worse. A person’s walking gets slower and less steady, leading to a higher risk of falls.
By the later stage of dementia, the condition will have a severe impact on most aspects of a person’s life. The person will eventually need full-time care and support with daily living and personal care, such as eating, washing and dressing. This support can be provided by care at home but is more often given in a care home setting.
Symptoms of all kinds are likely to cause the person considerable difficulties in this stage,
but altered perception and physical problems are often the most noticeable. By the late stage, the symptoms of all types of dementia become very similar.
Memory problems: They may often think they are at an earlier period of their life (known as ‘time shifting’). This can cause challenging situations, for example, if they ask to see someone who is no longer alive.
Language difficulties: If the person knows more than one language, they may lose one of the languages they learnt later in life. They will remember the language learnt in childhood.
A person’s spoken language may eventually be reduced to only a few words or lost altogether. They may also understand fewer words. But people with dementia at this stage may still be able to understand gestures, facial expressions and body language. They may also use non-verbal communication to express their feelings or needs.
Depression, apathy, delusions and hallucinations are most common. People with later stage dementia often respond more to senses than words. They may like listening to songs or enjoy textures. For example, they may like the feel of different types of material.
Aggression in the later stage of dementia is often a reaction to personal care. Someone may hit or push away those trying to help them or shout out to be left alone. The person with dementia may have felt scared, threatened or confused.
Restlessness is also very common. Sometimes the person may seem to be searching for someone or something or the person has some unmet needs. Someone with later-stage dementia will often be unable to tell others how they are feeling.
A sudden change in behavior can point to a medical problem (for example, pain, infection or delirium).
The physical changes of late-stage dementia are partly why the person is likely to need much more support with daily living. At this stage they may:
· Walk more slowly, with a shuffle and less steadily – eventually they may spend more time in a chair or in bed
· Be at increased risk of falls
· Need a lot of help with eating – and so lose weight
· Have difficulty swallowing
· Be incontinent – losing control of their bladder and bowels.
The person’s reduced mobility, in particular, raises their chances of blood clots and infections. These can be very serious or even fatal so it is vital that the person is supported to be as mobile as they can.
How long will a person with dementia live for? Whatever type of dementia a person has, their life expectancy is on average lower. This is why dementia is called a life-limiting condition. However, it’s important to remember that, no matter how a person’s dementia changes over time, there are ways to live well with the condition.
Good support can make a huge difference to the person’s quality of life at all stages of dementia.
The prognosis for dementia depends on the type of dementia and the age of diagnosis:
Alzheimer’s disease: The average life expectancy is 8–10 years, but it can be shorter if diagnosed in the 80s or 90s. A few people with Alzheimer’s live for 15–20 years.
Vascular dementia: The average life expectancy is around 5 years, but people with vascular dementia are more likely to die from a stroke or heart attack.
Dementia with Lewy bodies: The average life expectancy is around 6 years, but the physical symptoms increase the risk of falls and infections.
Frontotemporal dementia: The average life expectancy is around 6–8 years, but it progresses more quickly if mixed with motor neuron disease.
Median survival time: The median survival time from a dementia diagnosis is around 5 years.
Mortality risk: The risk of death increases with age, and is higher in men than women.
Contact Us
-
ALAMBANA Centre for Dementia Care
Plot No. 8-2-293/82/A/514, Road No. 10, Banjara Hills, Hyderabad – 500034 - ardsihyd@gmail.com
- 9121106681


